Shoulders are the most injured joint in your body. This is due to its unique and complex anatomy which gives the shoulder the most range of movement of all the joints in your body. Let’s break it down and simplify the shoulder.
Shoulders are the most injured joint in your body. This is due to its unique and complex anatomy which gives the shoulder the most range of movement of all the joints in your body. Let’s break it down and simplify the shoulder.
What is it?
The shoulder complex is made up of the humerus (upper arm bone), scapula (shoulder blade and clavicle (collarbone). The shoulder joint is a ball and socket joint between the humerus and scapula. The collarbone is attached to the shoulder blade and also plays an important role in shoulder movement. As the shoulder is a ball and socket joint it has a large amount of mobility. Being one of the most mobile joints in the body, it is more prone to injuries such as dislocations. The shoulder relies on the surrounding muscles to provide stability to the joint (in particular the rotator cuff and biceps).
What can go wrong?
Common injuries of the shoulder include:
- Rotator cuff tears/tendinopathies
- Subacromial bursitis
- Dislocation/subluxation
- Acromioclavicular joint injuries
- Frozen shoulder
If you are experiencing any shoulder pain, don’t hesitate to contact the clinic to book an assessment.
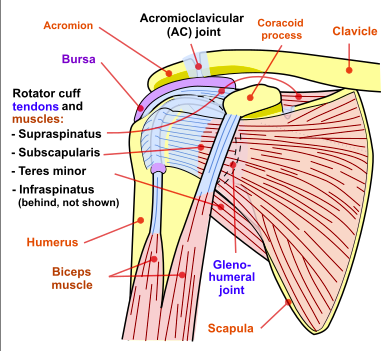
Image Source: National Institute Of Arthritis And Musculoskeletal And Skin Diseases (NIAMS); SVG version by Angelito7 – Shoulderjoint.PNG, Public Domain, https://commons.wikimedia.org/w/index.php?curid=29907860
Common Myths Debunked
#1 The Recipe for Good Posture is Pushing the Shoulders Down and Back
Ever been told to pull your shoulders back to get in good posture? Actually, jamming your shoulder blades together is really hard to maintain and can cause an overcorrection and end up with more tension in muscle in your neck. Instead try thinking ‘up tall’ and then let your shoulders fall naturally backward. This will be easier to hold for a longer time as it is a more natural position.
If your posture is poor from standing or sitting in long periods of time, imbalances can occur loading the ligaments and structures of the joints. If you are experiencing any pain or discomfort, a physiotherapist or exercise physiologist can help you get on the right track with your posture.
#2 I have a rotator cuff tear, I will need surgery
The rotator cuff is a group of 4 muscles that group together to form a ‘cuff’ around the top of the humerus (arm bone). It helps to lift and rotate the arm. A tear to the cuff can be caused from a fall or from repetitive use of the arm in a particular direction. Most small to moderate tears are managed without surgery through a rehab program to strengthen the rotator cuff and correct any issues that might be aggravating, like poor posture. Even though most tears cannot heal on their own, good function can be achieved without surgery.
However, surgery can be required with full thickness tears, and if you are actively required to use your arm overhead for work or sports.
#3 My scan says I have degeneration so that must be the cause of my pain.
So you have a sore shoulder and you visit your GP to question what the best course of treatment might be and to get the bottom of the problem you are sent for an X-Ray or MRI. The results show that you have degeneration of the rotator cuff, bursitis, or a tear and from then on this outcome is attributed to any pain that is experienced in the joint. The FACT is that there is a large chance that your symptoms ARE NOT the result of the findings on the scan at all because these findings can also be found in patients who are pain-free and undergo the same imaging! This means that the same results can show up on scans for people who have no pain and also those who are experiencing pain.
A study by Girish et al, 2011, found that in 51 people without any shoulder pain, 78% of them showed signs of bursal thickening, 65% ACJ degeneration and 39% showed cuff tendinopathy. In a separate study on 53 people without any shoulder pain, 72% of people were found to have SLAP lesions (Schwartzberg et al. 2016).
What does this mean? Well if you want to get to the route of your symptoms and reduce your pain, try seeing your physiotherapist first. They will assess you the same way whether you have a scan prior or not, and will provide treatment to relieve pain, strengthen and mobilise, and get you on the road to recovery.
In short, if you’re told you need a scan, query your health professional and in most cases, you could get away with saving your dollars by first seeing one of our expert physiotherapists!