The spine is a VERY complex part of the body. Here we try to simplify what it is and what can go wrong.
What is it?
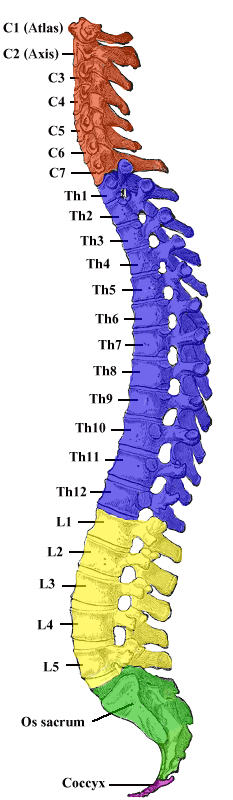
The spine consists of 4 sections: the cervical spine (the neck), the thoracic spine (the upper back), the lumbar spine (lower back) and the sacrum (tailbone). The cervical and lumbar spine both curve forwards (lordosis) while the thoracic spine and sacrum curve backwards (kyphosis). It is also normal to have a small amount of lateral (sideways) curvature of the spine, and each person’s spine will curve slightly differently. Different areas of the spine allow different levels of mobility. For example, there is a lot of mobility in the neck, less in the thoracic spine and then more in the lumbar spine, with very minimal mobility in the sacrum. When people have pain, it is usually in the transitions between these areas (for example between the lower lumbar spine and the sacrum which is the most common area for lower back pain).
What can go wrong?
Some conditions of the spine include:
- Osteoarthritis
- Acute or chronic non-specific low back pain
- Radicular pain or radiculopathy
- Compression fracture
- Wry neck
If you are experiencing any back pain, don’t hesitate to contact the clinic to book an assessment.
Common Myths Debunked
#1 I have a slipped disc
Fact: Discs don’t slip! Intervertebral discs sit between vertebrae in your spine. They are a fibrocartilaginous joint which allows movement between the vertebrae, acts as a ligament to hold the vertebrae together and act as shock absorbers. They are EXTREMELY STRONG structures, which are uniquely designed for their role. They are made up of an outer ring, with an inner gel like structure which helps to distribute pressure evenly across the discs and prevent excessive forces on the vertebral end plate (the top and bottom of the vertebrae). The vertebral end plates consist of both a bony and cartilaginous end plate which create an exceptionally strong connection to the disc, meaning that it cannot just slip out of place. One study looked at the tensile and compressive strength of thoracic discs in both younger and older populations. They found that it takes about 335kg of force to compress the disc height 1mm in young subjects and about 208kg of force to compress the disc height 1mm in older subjects.
#2 I blew out a disc and now it will never heal
Evidence shows that discs can heal and most have very high rates of healing depending on the individual and the particular pathology. A study by Chiu, et al looked at the ability of the intervertebral discs to heal. Depending on the injury the rate of spontaneous regression (spontaneous healing of the disc) was between 13-96%, with more severe injuries actually having higher rates of spontaneous regression. It is also important to realise that even though you may have an ‘abnormal’ finding on a scan, this is actually very common and it doesn’t mean that what you see on the scan is actually the source of pain. A study conducted by Hiroaki et al looked at scans of 1211 asymptomatic adults from age 20-80. They found that most participants had disc bulging (87.6%) which significantly increased with age. Even then, most participants in their 20s had bulging discs (73.3% of males and 78% of females).
#3 Moving will make my back worse
Bed rest is what used to be prescribed when someone had pain in their back. However, we now know that those who remain active will improve quicker, decreasing pain and improving their movement.
When the pain is new, it is important to find a balance between rest to let the pain reduce and keep moving even doing these movements in a different way will help. Just like if you have sprained your ankle and you limp around for a couple of days, if you stopped moving altogether the ankle would feel very stiff and painful when you start to move around again. It is exactly the same with the back. As your pain settles down, moving gets easier and you can get back to normal movement patterns.
Exercise has been shown through research to be the best treatment for pain. In fact, it is the only method of treatment to reduce recurrence of pain by 50%. So keep moving, no matter what it is, it will help!
Seeing a physiotherapist in the acute phase of injury will prescribe specific movements that will help to reduce pain.